Could you forget how to ride a bicycle?
That feeling of forward motion, untethered to a parent steadying the seat, stays with most people into adulthood. Hence the expression: You never forget how.
But imagine for a minute that you did have to forget. Could you unlearn something like that?
That’s what addiction is like, except instead of trying to unlearn something that is fun and mostly free of consequence, you’re trying to unlearn something that has the power to take over your life.
Or to kill you.
Dr. Ruben Baler, a neuroscientist with the National Institute on Drug Abuse, said there are many metaphors to explain addiction, but he’s partial to the bike-riding analogy.
“One of my hopes has been that if you can just get people to understand the science, the stigma would just melt away,” Baler said in a telephone interview from NIDA’s headquarters in Bethesda, Maryland. “That hasn’t really happened though.”
The science of addiction is complicated. It’s easier for people to see it as black-and-white. A person makes bad choices and has to live with them. Or, a person started using these drugs, so they can stop; it just takes willpower. This line of thinking is persistent, and even understandable, but researchers say it impedes progress in slowing down the drug crisis.
“Every drug of abuse from the moment of the first use, changes the wiring and connectivity of the brain,” explained Vivek Kumar, a researcher at The Jackson Laboratory in Bar Harbor who studies the genetics of addiction. Opioids are particularly problematic, though, because of the speed at which they can take over the brain.
‘DOPE SICK’: THE WORST FLU IMAGINABLE
But how does that happen?
Inside the brain are numerous receptors, tiny sites where chemicals, natural or otherwise, bind during neurotransmission.
When the brain feels pleasure, it’s because the body releases chemicals such as dopamine, which attach to receptors. Opioids stimulate a large release of dopamine for the purpose of alleviating pain.
Ask someone to describe the first time they used heroin and the responses are almost romantic. It’s an overwhelming sensation of warmth and safety. It’s like being wrapped in a gentle euphoric hug.
But opioids also bind to other receptors not related to the reward system. Over time – and it doesn’t take long – the brain adapts to these changes in neurotransmitters so that they function normally only when opioids are present.
Even activities that increase dopamine production naturally – things like exercising, eating certain foods, even listening to music – are shunted aside.
“One thing about opiate addiction that stands out is how much a driving force avoidance of withdrawal is,” said Emily Feinstein, director of health law and policy at The National Center on Addiction and Substance Abuse. “Withdrawal then becomes a deterrent to stop.”
Users call it “dope sick,” and their description of it is grim: the worst flu imaginable, amplified by a power of 10. Those suffering from opioid addiction never get back the same feeling of that first high but they are always chasing it.
Here’s another metaphor: If you’re starving, because you haven’t eaten in three days, and your mind is starting to hallucinate, what would you do to find food? Might you do something risky or potentially harmful to satiate that hunger?
Many people suffering from addiction say that they became a different person while using. Loved ones say the same thing. I didn’t recognize my son or daughter anymore, they say.
GENETICS, ENVIRONMENT PLAY A ROLE
This is why.
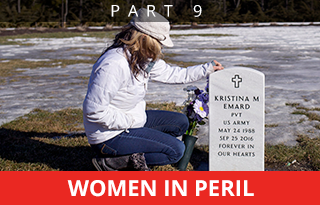
Heidi-Sue Stuart lost her son to heroin in November 2015, but the young man she knew was lost to her long before that. Things changed drastically after a car accident in 2009 left Corey Coburn with severe facial injuries. He had six different plastic surgeries. A metal plate was inserted around his eye. His jaw was wired shut for eight weeks.
Stuart said she slept in the same room with her son for a while because the pain scared him so much.
His doctors prescribed several painkillers: morphine, Percocet, then OxyContin. Six months in, doctors tried to wean him down from high doses with Suboxone.
But Suboxone wasn’t enough. Coburn’s brain had been rewired.
“After the accident you could tell the change. He was angry all the time. He was irritable. He seemed overwhelmed. He seemed stressed,” his mother explained. “Then you would see him relieved. I think he was taking whatever he could to just get by.”
“I know it’s true, myself included, when you think of a heroin addict you think of someone in the alleyway and you don’t think of it being someone close to you and someone you love.”
VITAL SIGNS: Fatal drug overdoses in Maine climbed by 80 percent in the last three years — from 208 to 376.
Baler, the NIDA neuroscientist, said the effects of opioids on the brain are relatively easy to explain, but what complicates addiction is what drives a person to misuse in the first place or why some people are more prone to addiction than others.
No single factor can predict whether a person will become addicted, but genetics and the environment play a role. Poverty, abuse in the home, unstable parents – those are all risk factors.
“The multidimensional aspects of addiction put it in the same family as other psychiatric disorders,” Baler said. “That’s why it makes so much sense to have a multipronged approach to treatment.”
‘WE NEED TO GO WHERE THE EVIDENCE IS’

Vivek Kumar, a researcher at The Jackson Laboratory, said it’s hard for him to watch so many people lose their lives to addiction, knowing that science explains how to treat it.
He said medication-assisted treatment like Suboxone or methadone helps to stabilize the brain to make it possible for long-term behavioral recovery.
The key is long-term. It’s so much easier for the brain to learn than to unlearn. Think back to riding a bicycle. Where would you even start to unlearn that skill?
That’s why it’s so important to think about addiction as a brain disease when thinking about treatment and recovery, Feinstein said.
“Abstinence-only is often not successful because the brain hasn’t recovered,” she said. “We still sort of have this approach of you go to a provider and they have one kind of treatment, sort of like how we treated cancer a while ago.
“But everyone is different. If you don’t give the person the treatment that matches their disorder, the success rate is not going to be high.”
Relapse, which happens for as many as 60 percent of opioid addicts – sometimes more than once – often is a clear sign that more or different treatment is needed. But many treatment programs still view relapse as failure.
Even within the treatment community, there is a lot of bias and stigma – the same attitudes carried by those who suffer from addiction.
Abstinence-only advocates may take the position (even unintentionally) that a patient can’t be fully “clean” while on a methadone or Suboxone maintenance program, thereby closing off a scientifically proven form of addiction treatment.
Supporters of medication-assisted treatment, on the other hand, may rely too much on the medicine and not the behavioral therapy that is paired with it, leaving patients with a long-term reliance on the medication because they haven’t gotten to the root of why they used in the first place or because they haven’t learned the skills to suppress urgings or cravings.
Kumar, the Jackson Lab researcher, said if the goal is to help people suffering from addiction, “We need to go where the evidence is.”
The evidence, according to scientists, is medication-assisted treatment coupled with behavioral therapy.
But it’s not a magic bullet. It is work and it can be costly.
Kumar said it’s hard for him to watch so many people lose their lives to addiction, especially knowing that just as science explains addiction, it also explains how to treat it.
“I’m safe in my lab writing grants and doing work. I’m dealing with mice,” he said. “But I do think that, after all these years of waging a war on drugs, we have a real opportunity to get this under control.
“But will we? I don’t know.”
This story was updated at 4:09 p.m. April 13, 2017 after the Maine Attorney General’s Office revised its preliminary estimate of the number of drug overdose deaths in 2016.
Eric Russell can be contacted at 791-6344 or at:
Twitter: PPHEricRussell
Send questions/comments to the editors.





















Comments are no longer available on this story