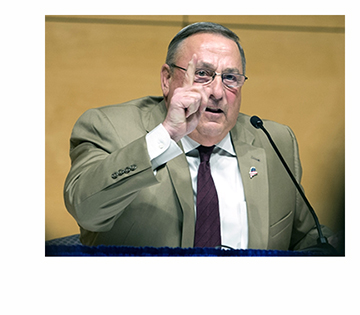
Gov. Paul LePage went to Portland on Tuesday and took questions from a live audience. When thrown what should have been an easy question, however, the governor blew it badly.
LePage was talking about the state’s response to a dramatic increase in heroin traffic and overdose deaths. He was defending his decisions on funding for drug treatment when Andrew Kiezulas, a recovering addict who served on former Mayor Michael Brennan’s drug task force, asked:
“Does treatment work, Mr. Governor?”
“Not with heroin,” LePage answered. He said a majority of addicts wash out of state treatment programs, and the money spent on programs is largely wasted.
“Treatment is fine,” he said. “Some people are willing to be treated and some aren’t. We cannot force people to be treated. … You have to want it.”
That exchange clearly illustrated why LePage and the Legislature have been fighting over the right approach to address the epidemic of opiate addiction and overdoses instead of uniting behind an approach that would save people’s lives. Lawmakers have supported a multi-pronged approach that would interrupt the illegal drug supply chain with added resources for law enforcement, while suppressing demand for dangerous drugs with additional treatment and education.
LePage has backed a purely law enforcement approach, and on Tuesday, it became clear why. He doesn’t think treatment works. He could not be more wrong.
Scientists looking at decades of data show overwhelming results from the right kind of treatment.
The gold standard for heroin addiction treatment is methadone maintenance. Methadone is an opiate that is formulated to prevent withdrawal and cravings, but when used correctly, will not intoxicate the patient. Addicts on methadone have an 80 percent success rate while participating in a program, and are able to hold jobs and lead normal lives.
Their rates of infection from HIV and other blood-borne diseases decrease dramatically, and so do their rates of overdose and death. That’s only when they are on the program, however. When they are forced to wean off methadone, most former patients relapse within a year.
There is less of a track record for buprenorphine, but addiction specialists say that can be just as effective for some patients. It has the added benefit of being distributed by prescribing physicians, and it doesn’t have to be administered in a clinic setting, like methadone.
Pharmaceutical treatment is not perfect, and it doesn’t work for everyone. But it does work.
What doesn’t work is denying treatment to people who need it — and a lack of health insurance coverage is what keeps people from getting life-saving care.
Maine has the highest rate of people without health insurance in New England, a direct result of state policies since LePage came to office in 2011. As the other states in the region were expanding eligibility for their Medicaid programs, Maine was restricting ours. Maine not only refused to accept a federally funded expansion that would cover people with incomes slightly above the poverty line, but also stopped covering childless adults with incomes below the poverty line.
And even people still covered by MaineCare have a 24-month lifetime cap for treatment with methadone or buprenorphine. Once the cap is reached, people who had been given a chance to manage their addiction are left to fend for themselves.
The governor needs to know that it’s not treatment that doesn’t work — it’s denying treatment to people who need it that is a recipe for failure.
Maine is not going to fight its opiate crisis with policymakers at such a high level who have a fundamental lack of understanding of the tools that are available. We hope that the Legislature can work around the governor and reach a bipartisan consensus on expanding law enforcement, education and treatment approaches to opiate addiction that will save lives.
Send questions/comments to the editors.